Interpersonal Communication in Healthcare
Interpersonal communication skills are always important in healthcare, but especially now as the U.S. faces a mental health crisis during the COVID-19 pandemic. In a recent MMWR, the CDC reported that symptoms of anxiety disorder and depressive disorder increased considerably in the United States from April to June of 2020, compared with the same period in 2019. They recommend that “the public health response to the COVID-19 pandemic should increase intervention and prevention efforts to address associated mental health conditions.”
“The public health response to the COVID-19 pandemic should increase intervention and prevention efforts to address associated mental health conditions.”
– CDC, Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic
Keep reading to learn more information about interpersonal communication in healthcare, why and to which populations it’s especially important for now, and how healthcare professionals can improve essential skills.
What is Interpersonal Communication and Why Does it Matter in Healthcare?
One study defines interpersonal communication in healthcare as “the ability of the provider to elicit and understand patient concerns, to explain healthcare issues and to engage in shared decision-making if desired.” It’s more than just what you say—though that is a big part of the puzzle. It’s also how you say it, and what you mean by it.
Numerous studies have linked interpersonal communication in healthcare to improved patient outcomes, including:
- Higher patient satisfaction
- Improved adherence to treatments
- Reduction in psychological effects (depression/anxiety)
- Increased patient confidence or self-efficacy
- Symptom reduction
- Improved quality of life
- Increased survival rates
These outcomes—which range from short-term to long-term—are extremely significant. Strong interpersonal communication skills can help save lives and help people live longer, which is why it’s such an important topic in healthcare.
Interpersonal Communication in Healthcare for At-Risk Patients
The recent CDC MMWR report reveals considerably elevated adverse mental health conditions associated with COVID-19. Overall, over 40% of adults reported at least one adverse mental or behavioral health condition. Younger adults, racial/ethnic minorities, essential workers, and unpaid adult caregivers reported having experienced disproportionately worse mental health outcomes, increased substance use, and elevated suicidal ideation.
As government stay-at-home orders are relaxed, these patients are beginning to seek routine medical care again. The medical community is on the frontlines and can play an essential role in helping patients who may be struggling with mental health or substance use disorders.
Medical professionals are not necessarily behavioral health professionals, but more institutions are integrating behavioral health into primary care with training. By acquiring the knowledge and communication skills to confidently perform screenings for mental health conditions and substance use disorders—such as SBIRT (screening, brief intervention, and referral to treatment)—healthcare professionals can help patients achieve better long-term health outcomes.
Interpersonal Communication for Every Patient
Patients and families are under severe stress, whether or not they are suffering with mental health or substance use disorders. A recent review from samples of quarantined people showed numerous emotional outcomes, including stress, depression, irritability, insomnia, fear, confusion, anger, frustration, boredom, and stigma associated with quarantine, some of which persisted after the quarantine was lifted. Feelings of uncertainty, financial hardship, and uncertain prognoses can also contribute to widespread distress.
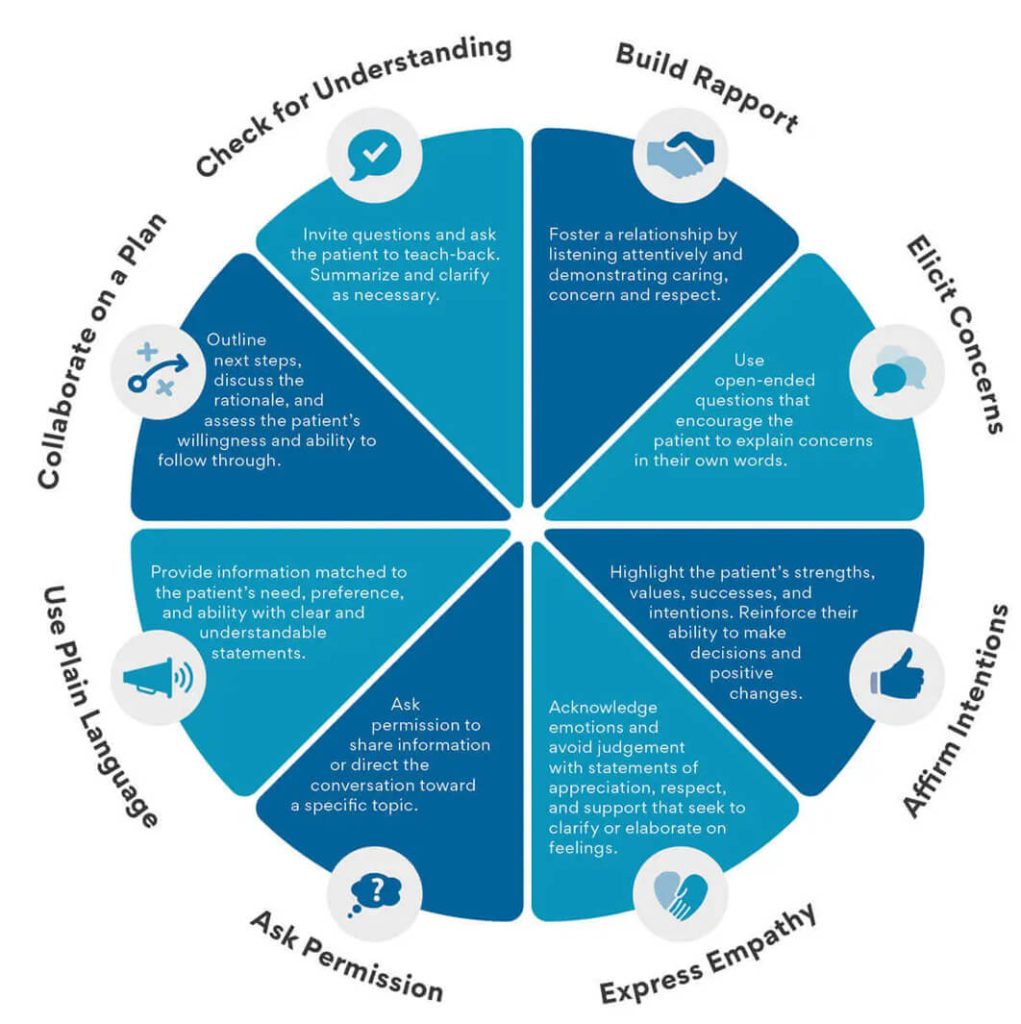
Interpersonal communication in healthcare can help make a difference during this sensitive time, and can lead to better patient satisfaction and even outcomes. Skills in the diagram below—such as clear communication and expressing empathy—are important when treating any patient, especially during the COVID-19 pandemic when stressors are high.
Interpersonal Communication Can Help Healthcare Professionals Facing Burnout and Stress
Healthcare professionals are certainly not immune to the widespread stress. A new NC State study found that healthcare workers are actually at greater risk than the general public of experiencing health problems such as depression. Many are facing the coronavirus on a daily basis, may have experienced trauma during an outbreak, and could be overwhelmed by fear of infecting themselves or loved ones.
Even before the COVID-19 pandemic, many healthcare workers already suffered from work-related burnout or depression. A third of U.S. nurses felt unengaged or burned out at work, and emergency medical services workers developed post-traumatic stress disorder at nearly double the rate of the general population. The pandemic only exacerbates these issues, and interpersonal skills in the workplace are important as healthcare workers look out for one another.
Interpersonal communication in healthcare is actually proven to combat burnout and stress. Poor team communication has been directly linked to high turnover rates and low morale. Developing skills such as empathy, collaboration, and relationship-centered communication can strengthen healthcare teams and promote a more supportive and positive work environment.
Strengthening Telemedicine With Effective Interpersonal Communication
As telemedicine becomes more widespread, there’s a need for healthcare providers to develop good “virtual bedside manner”.
Although there is physical distance in virtual appointments, there’s still a need to connect to the patient and develop trust. When you consider that up to 93% of the emotional meaning of messages is communicated nonverbally (such as facial expressions), the fact that providers can communicate with patients virtually without a mask covering could actually be seen as a better opportunity for connection. Developing strong communication skills can help make telemedicine appointments more positive and effective.
If you’re a healthcare provider or educator looking to strengthen essential soft skills, Kognito now offers role-play simulations that build interpersonal communication skills in healthcare. These simulations train providers to apply evidence-based communication skills that enhance patient engagement, reduce time spent with clients, and improve health outcomes. Learn more and access a free demo of our interpersonal communication in healthcare simulations here.
- Using Simulation-Based Education to Fulfill Clinical Hours
- Motivational Interviewing: Approaches You Can Use Today
- Scaling Mental Health and Substance Use Training for Health Professionals
- Meeting the Quadruple Aim with Simulation Technology
- The Case for Doctor-Patient Communication to Improve Healthcare Quality